The president has got to make a decision.
Blue City Lockdowns Obscure COVID’s Root Causes

We can be far more efficient in our fight against pandemics.
It will be months, likely years, before we understand how COVID-19 has reshaped our communities. Yet there is enough data, based on just the last three months, to get some notion of what areas and populations are most vulnerable.
The patterns are in many ways fairly clear. Media outlets, particularly those based in New York, seem to feel that the pain of the urban centers will be shared universally. The “science” as generally endorsed by our ruling Clerisy dictates that we impose strong controls which, though perhaps necessary in New York and other places, have been disastrous in marginally unaffected rural and suburban areas.
In reality, the data seem to indicate that exposure density, mass transit, and poverty are the key factors in facilitating the spread of the virus. Targeted attention to those areas would constitute a far more efficient and effective response than the one our elites are currently forcing upon us.
The Density Connection
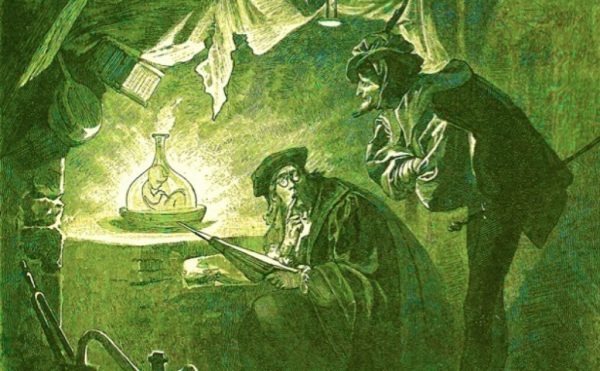
Perhaps no aspect of the pandemic’s rise has been more hotly contested than population density. Yet the tie between density and pestilence is not a new one. It is reminiscent of great Renaissance cities like Venice which, as noted by historian William McNeill, suffered grievously from waves of pestilence far more than relative backwaters in central Europe and Poland. Then and now, many of the same things that make cities great—such as exposure to foreign trade and immigrants—naturally aid the spread of pandemics. Most of the largest hotspots for COVID-19 to date in both America and Europe have been dense, urban areas.
Technically speaking, it is not population density per se that matters so much as what is called “exposure density”—that is, the amount of time spent in unavoidable close proximity to others, particularly in unventilated spaces and crowded households. But population density, of course, is a major factor of exposure density. This likely explains, to a large extent, the extraordinary rate of infection and fatalities located in New York City and some of its suburban areas. The city itself represents only 2.5% of the nation’s population, yet accounts for 15% of cases and an astounding 26% of fatalities, according to the Johns Hopkins virus dashboard (May 7).
Apologists for dense urban development point to the relative success in containing the contagion in places like Singapore, Tokyo, and Seoul. These cities have benefited from their experiences with previous pandemics such as SARS; they enjoy less extreme poverty; and their populations are generally more disciplined and less diverse. Even so, all are now facing a new upsurge of cases. In Japan, 30% of all cases are in Tokyo prefecture—this is nearly three times the prefecture’s share of the country’s total population. As a result, Japan has been forced to go back under lockdown as its hospital system becomes increasingly stressed.
The geographic differentials are equally stark in the United States, which was clearly far less prepared for the pandemic. New York is home to some of the densest neighborhoods in the nation and remains by far the most transit-dependent city in North America. Life is just much more crowded in the city, which makes social distancing more difficult, lockdowns more draconian, and exposure density more severe.
Unsurprisingly, the media, based as it is largely in New York, warns that the rest of the country faces the same or similar risk of infection. This may be true, but there is not much evidence now. Less urban states like Iowa, Nebraska, and South Dakota now all have among the lowest rates of COVID-related deaths in the country—roughly one fortieth that of New York. These divisions have been so widespread that some states have tried to keep people from high-infection areas from entering.
Economist Jed Kolko estimates the death rates in large urban counties to be well over twice those in high-density suburbs and four times higher than those in lower-density ones, with even larger gaps between smaller metros and rural areas. These findings are largely confirmed by the research of the Brookings Institution. According to data published by the New York Times, the Empire State has had a fatality rate more than 40 times that of Texas, and about 20 times that of California and Florida.
Transit and Exposure Density
Another key multiplier for exposure density is transit. People who spend a long time each day packed on commuter trains and subways are clearly more vulnerable than those who work at home, or ride in cars. This is particularly evident in New York City (home to nearly 30% of nationwide transit commuters), as MIT medical economist Jeffrey Harris shown. That situation was made particularly bad, at least in the early days of the pandemic, by Mayor Bill de Blasio’s almost diabolical call for New Yorkers to ride the subways without fear. But crowded public transportation is also a factor in limited areas like Detroit, a generally weak transit market where many poor people take the bus.
In contrast, areas with greater car usage—like Dallas-Ft. Worth, Houston and even Los Angeles—have had dramatically fewer cases and fatalities. For example, Dallas County has 60% more residents than Manhattan, but at least 90% fewer fatalities. Houston’s core Harris County has three times the population of Manhattan and also at least 90% fewer fatalities. Los Angeles County has 20% more residents than the city of New York, yet also has at least 90% fewer fatalities than NYC. At the same time the rate of infections in nearby Orange County, where car usage is even greater and single family homes more prevalent, is barely one seventh of that in Los Angeles County.
Perplexingly, some transit advocates are doubling down on their advocacy of both more density and more transit, despite the clear implications of the data. One economist even traces the extraordinary outbreaks in the outer boroughs to people driving cars—this despite the fact that most commuting there is by transit. Some environmentalists even see in the lockdown a “test run” for their proposals to achieve “de-growth”—these fans of the lockdown go so far as to celebrate the empty city streets (lined as they are with bankrupt and abandoned stores). But it is hard to see how cities can practice social distancing if they become more dependent on transit usage rather than less.
A Big Issue: Poverty
Arguably one of the biggest and least-understood vectors for this virus is poverty. Dense urban pockets of wealth like Manhattan or San Francisco have done relatively well. The wealthier have more options—such as drivers, rideshare services like Uber, and cabs. They can afford to avoid their workplaces, or else their commute may be walkable. Others can retreat to their country houses or work at home. In contrast, working-class people in city hotspots have little choice but to use crowded subways and buses. They often work and live in conditions of extreme exposure density.
Poor people in general also often have limited access to health care, even though they disproportionately suffer from diabetes, obesity, and other ailments. These same preconditions have made them particularly vulnerable to the virus. This can be seen not only in New York or Detroit but also in some ski resorts, meat-packing plants, and Native American reservations. There are concerns that some impoverished rural areas could be added to this list. Ultimately, there can be no useful response to future pandemics without addressing the predicaments of poverty in the U.S.
Whether in New York, Detroit, New Orleans, Houston, or Los Angeles, the brunt of the infection—outside of nursing homes—seems to be in poor neighborhoods. In both New Orleans and Detroit, the vast majority of deaths have been Americans. This is not a diminishing problem: Despite all the brouhaha about urban renaissance, the number of these high-poverty areas has grown steadily over the past few decades and doubled in population between 1980 and 2018.
Generally, poor people are more transit-dependent than the wealthy. New York reveals that it is not the posh Manhattan high-rises that have been hardest hit, but dense, transit-dependent, and working-class areas in central Queens (home to New York’s largest Chinese community), crowded eastern Brooklyn, and the impoverished Bronx.
But poor people’s exposure density is more than simply a function of transit or crowded work sites. Many suffer from exposure density in their everyday lives and are far more likely to live in crowded apartments and ride crowded elevators. They also often live in multi-generational households because of economic constraints. In the outer boroughs with subway service (the Bronx, Brooklyn and Queens), households are 3.5 times as likely to live in apartments as in houses. Similarly in Los Angeles, where infections have clustered mostly in the poor south, we again find crowded households.
Arguably even more affected will be a new generation of workers who, having been clipped by the Great Recession, now are suffering the largest share of the job losses. It is the low-income worker, more than any segment of society, that is bearing the biggest burden from the lockdowns.
Where We Go from Here
To survive, cities need to focus on reducing exposure density, which the public may also support. Right now, according to the Harris Poll, as many as two in five urban residents, including the young, are considering a move to a less dense place. The latest consumer survey from the National Association of Realtors found consumers are “looking for larger homes, bigger yards, access to the outdoors and more separation from neighbors.”
The cities of the future will no doubt retain “hip”, dense creative districts, but tech and high-end business services have been moving during the past five years to sprawling, low-density metro areas like Austin, Nashville, Orlando, Charlotte, Salt Lake City, and Raleigh. For many cities, it might make sense to give incentives not for office towers but for home-based workers; most people now working from home—some 60% according to Gallup—express a preference to continue doing so for the foreseeable future.
For the rest of the population, the last thing we need is another economic collapse as deep as a depression, which, even if it is short, will produce millions of “losers” who will never recover their lives. Rather than adhere to the ideological visions of planners and pundits, we need to move in bold ways to minimize potential exposure to this and future pandemics.
This should largely be led by the marketplace and through innovation. Consumers will demand new alternatives to transit, going beyond telecommuting to autonomous cars and cabs, which could provide mobility in the niche areas where transit dependence is high. Consumer demand could lead to changes in housing design, for example, such as developing houses with separate entrances and dedicated workspaces.
Faced with a crisis in urban forms, the biggest danger would be to do nothing, or even double down on the very things that worsened the pandemic. Density, transit, and poverty present special challenges in the pandemic era. Finding ways to address them should be our highest priority for the future.
The American Mind presents a range of perspectives. Views are writers’ own and do not necessarily represent those of The Claremont Institute.
The American Mind is a publication of the Claremont Institute, a non-profit 501(c)(3) organization, dedicated to restoring the principles of the American Founding to their rightful, preeminent authority in our national life. Interested in supporting our work? Gifts to the Claremont Institute are tax-deductible.
How all-too-human scientists have opened the door to pandemics—and worse.
Donor dollars shouldn’t be made in China.
Defective standards in social distancing.
Republicans need a new mission.
American voters will decide if the PRC wins.